Huffington Post has published a
discussion Joel Nitzkin and I had with psychotherapist Robi Ludwig (here). HuffPo was
not able to use the large number of resource links we provided, so I am
republishing the article with the full complement, below.
Two Doctors on A Mission to Set the
Record Straight about Smokeless Tobacco and Its Impact on Public Safety
By
Robi Ludwig, PsyD, Contributor
The historical roots of tobacco go way back to almost the beginning of time. Some date it
as early as 1 B.C. when the American Indians used it for religious and
medicinal practices. Given what we know about tobacco today it’s almost
impossible to believe tobacco was ever thought of as a cure-all for everything
from dressing wounds to the standard go-to painkiller.
By the 1600’s tobacco was so popular
that it was even used almost as frequently as money. Some even referred to it
“as good as gold”.
But some of the dangerous effects of
smoking tobacco was starting to become apparent during this time, too. Sir
Francis Bacon, the 1st Viscount St Alban, an English philosopher, statesman, scientist,
jurist, orator, and author, who served both as Attorney General and as Lord
Chancellor of England, admitted to having a very hard time quitting his tobacco
use and found it to be an impossible “bad” habit to break.
When we fast forward historically to
the 1960’s, this is when the Surgeon General reported the various dangers of
smoking to our health. And by 1971 Commercial Ads for cigarettes were taken off
the air in the United States as an attempt to curb this dangerous and growing
habit.
Even today, with everything we know
about the dangers of smoking, there are still some misperceptions out there
about tobacco use, which could negatively impact up to 8 million adult American
Smokers, but not if two prominent doctors have their way.
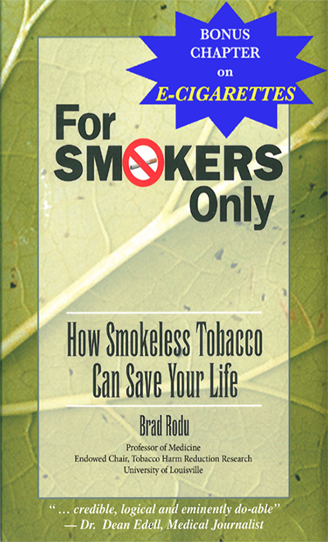
Now Dr. Rodu and Dr. Nitzkin are trying
to influence the public about Tobacco use by setting the record straight. Dr.
Brad Rodu, who has studied the science behind tobacco harm-reduction strategies
and has been appointed the first holder of the endowed chair in tobacco harm
reduction research at the University’s James Graham Brown Cancer Center and Dr.
Joel Nitzkin, public health physician, who is board certified in preventive
medicine and has been involved in tobacco control activities since the late
1970’s, have made it their professional mission to reduce tobacco-related
illnesses.
Dr. Rodu and Dr. Nitzkin strongly
believe that smokers who are unable or unwilling to quit cold turkey should be
informed about much lower risk smokeless tobacco or e-cigarettes. I spoke with
both doctors to find out how they believe adult smokers can potentially be
spared from life-threatening smoking-related illnesses. Here’s more about what
they both had to say on this topic.
Dr. Robi: What exactly is smokeless
tobacco, why was it created?
Dr.
Rodu and Dr. Nitzkin: Anthropologists and historians believe that tobacco has
been used by humans for thousands of years.
The plant originated in the New World and was completely unknown outside
the Americas until 1492, when Columbus first encountered native Americans using
tobacco for ceremonial and medicinal purposes.
They smoked and chewed tobacco, the latter serving as the provenance of
modern smokeless tobacco products.
Smokeless tobacco dominated the American market prior
to the 20th Century, because a day’s supply could be carried and
conveniently used in both industrial and agricultural work settings. In contrast, smoking was uncommon because
producing cigars, cigarettes and pipes was labor-intensive and expensive. In addition, smoking was very inconvenient
before a safe and portable source of fire was readily available, which didn’t
happen until the widespread use of safety matches in the late 1800s.
Dr. Robi: What are the different kinds
of smokeless tobacco?
Dr.
Rodu and Dr. Nitzkin: In the U.S. there are two main kinds of smokeless
tobacco. Loose leaf chewing tobacco
(“chew”) consists of shredded tobacco leaves and stems packaged in foil
pouches. Chew is also heavily sweetened
and flavored. It is used in fairly large
quantities, which produces the typical swollen cheek appearance and generates a
lot of juice.
Moist
snuff, also called dip tobacco, is the most popular smokeless product in the
U.S. It is manufactured from dark,
fire-cured tobaccos grown in western Kentucky and Tennessee, fermented and
ground to the consistency of finely chopped parsley. Multiple flavors are available, but moist
snuff does not contain sweeteners. It is
used in small amounts, generally as much as can be grasped between the thumb
and forefinger in a “pinch.” The tobacco
is then placed inside the lower lip between the cheek and gum.
Moist
snuff is hard to contain in one spot, so manufacturers have packaged
pinch-sized portions in small tea-bag type paper pouches. The pouches are no larger than a piece of
chewing gum or a breath mint, making them virtually invisible to place and
use. They also don't disintegrate, which
makes the tobacco easy to remove after use.
Since
2005 a Swedish version of moist snuff, called snus, has become more popular in
the U.S. Rather than fermented, the
tobacco is treated by a pasteurization process that gives it a different flavor
than American dip, and somewhat lower levels of unwanted contaminants. Snus is also marketed in many flavors and
small pouches.
Americans
place moist snuff in the lower lip, where it generates juice and spitting. In contrast, Swedes don’t have to spit when
they use snus, mainly because they place it inside the upper lip.
Nicotine
is absorbed from all smokeless tobacco products through the lining of the
mouth, giving the user a “buzz” very similar to, but with a slower onset than
that achieved by smoking a cigarette.
Nicotine is not the major cause of any disease; it is no more harmful
than caffeine, which is also addictive but safely consumed in coffee, tea and
cola drinks.
Dr. Robi: Are different kinds of
smokeless tobacco better for you than others?
Dr.
Rodu and Dr. Nitzkin: No tobacco product is absolutely safe. All contain traces of unwanted contaminants
in addition to nicotine.
But it’s been known for two
decades that, by avoiding smoke, chewers, dippers and snusers eliminate about 98% of the health risks associated with smoking. The risks are so small that even large
epidemiologic studies with hundreds of thousands of users cannot provide
indisputable evidence that smokeless tobacco causes any disease.
With
risks that small, it is not possible to prove that one kind of dip, chew or snus is
safer than the other.
Dr. Robi: Why is there so much
confusion about smokeless tobacco and if this is a healthy alternative to
regular cigarettes?
Dr.
Rodu and Dr. Nitzkin: Decades of scientific studies document that smokeless
tobacco use is vastly safer than smoking with respect to cancer, heart attacks and strokes and many other diseases.
There is no confusion about smokeless tobacco
among tobacco research and policy experts.
In 2002 a report by the British Royal College of
Physicians, one of the world’s oldest and most prestigious medical societies,
stated “As a way of using nicotine, the consumption of non-combustible
[smokeless] tobacco is on the order of 10-1,000 times less hazardous than
smoking, depending on the product.” The
Royal College issued another report in 2007 concluding “…that smokers
smoke predominantly for nicotine, that nicotine itself is not especially
hazardous, and that if nicotine could be provided in a form that is acceptable
and effective as a cigarette substitute, millions of lives could be saved. In 2008 the American Association of Public
Health Physicians became the first medical organization in the U.S. to formally adopt a policy of “…encouraging and enabling
smokers to reduce their risk of tobacco-related illness and death by switching
to less hazardous smokeless tobacco products.”
Cigarettes
are so popular that tobacco controllers incorrectly use the terms “smoking” and “tobacco use”
as if they were synonyms, and they have become obsessed with the notion of a
tobacco-free society. They have
transformed a legitimate war on smoking into a moral crusade against all
tobacco products, a mistake that was tragically made with alcohol almost 100
years ago.
When
a federal survey asked in 2015 if smokeless tobacco products are less hazardous
than cigarettes, only 11% correctly answered “yes”; 67% responded “no” and 22%
didn’t know. In other words, 89% of
Americans have no clue that dipping, chewing and snusing are
98% safer than smoking. They are
confused because they have been misinformed for decades by government agencies
and medical organizations that all tobacco products are equally harmful.
Misinformation
from public health officials should no longer be tolerated. Recently, two internationally renowned
tobacco policy experts, Lynn Kozlowski, professor at the University of Buffalo
School of Public Health and Health Professions, and David Sweanor, adjunct
professor of law at the University of Ottawa, urged the FDA to end a $36 million campaign against
smokeless tobacco “that fails to directly warn about the much greater harms
from smoked tobacco (predominantly cigarettes).” They concluded that “Public health agencies
have an obligation to correct the current dramatic level of consumer
misinformation on relative risks that they have fostered.”
Dr. Robi: Why do you think the FDA has
not informed the public about the whole truth about smokeless tobacco?
Dr.
Rodu and Dr. Nitzkin: Obsessed with the notion of a tobacco-free society, the
FDA so far has taken a hard line, falsely claiming that “To date, no tobacco
products have been scientifically proven to reduce risk of tobacco-related
disease, improve safety or cause less harm than other tobacco products.” In other words, no tobacco product is
absolutely safe. The agency is defying a
key element of its stated mission – “to provide the American public with
factual and accurate information about tobacco products.” And Congress in 2009 prohibited tobacco
companies from any communication with smokers regarding safer smokeless
alternatives without the express approval of the FDA.
The
FDA has refused to acknowledge that its smokeless warnings are inaccurate.
Even worse, some of its regulations threaten to remove large numbers of smokeless and vapor products from the market. In some cases the regulations require
companies to conduct dozens of unnecessary studies on minute product details
and human effects, which could take a decade or more.
This
is regulatory fundamentalism, a bureaucratic maze that condemns smokeless
tobacco products and e-cigarettes, and therefore tobacco harm reduction, to
purgatory. With this delay, cigarettes will continue to dominate the American
tobacco market, and 440,000 Americans will die from smoking-related disease
every year.
Dr. Robi: How many adult smokers use
smokeless tobacco as a way to quit smoking altogether?
Dr.
Rodu and Dr. Nitzkin: Federal surveys are usually used to count current, former
and never tobacco users. The surveys
generally don’t ask former smokers if they switched, but there was one
exception. In 2000, the National Health
Interview Survey asked former smokers if they had quit by switching to
smokeless; some 260,000 men said yes, providing the first population-level evidence that smokeless is a viable cigarette
substitute.
The
2015 NHIS documented that there were 5.1 million current smokeless tobacco
users that year. Unfortunately, the
survey didn’t ask former smokers specifically about switching, but about 1.6
million smokeless users were former smokers, meaning they had switched to safer
products like dip, chew or snus. Almost
1.4 million smokeless users were current smokers; if they were made aware that
smokeless was 98% safer, they might have fully switched.
Dr. Robi: How many smokers die every
year from smoking cigarettes? How about from smokeless tobacco?
Dr.
Rodu and Dr. Nitzkin: According to the CDC, the annual death toll among smokers is 440,000.
Despite the fact that smoking rates have been plummeting for three
decades, the CDC death toll hasn’t changed for nearly 20 years. In 2013, an FDA scientist concluded that the CDC estimate is too high.
One
might assume that the CDC tracks smoking deaths throughout the year, but that’s
not the case. Instead, they estimate the
number of smokers in the U.S., then they apply secret mathematical formulas
based on comparisons between current, former and never smokers. A reporter years ago tried unsuccessfully to
crack the black-box formulas. Here is
her summary: “The computer is fed raw data and...
employs various complex
mathematical formulas to
determine how many people in various age groups, locations,
and heaven knows what other categories are likely to get sick or die from what
diseases and how many of these can be assumed to be smoking related.”
The
CDC provides death counts among smokers with single-digit precision (the
current number is 439,033), but when it comes to deaths from
smokeless use, the agency claims it can’t be done.
In fact, the CDC has the necessary data; its disinclination is likely
due to the very low number that would result.
British researchers are not so inhibited; they reported in 2015 that there were no cancer
deaths due to smokeless tobacco in the U.S. and Canada. Last year, U.S. government-sponsored research
revealed that the number of mouth cancer deaths among men who use dip or chew
is zero.
Dr. Robi: What is the “Swedish
Experience” and how does it connect to tobacco harm reduction?
Dr.
Rodu and Dr. Nitzkin: In virtually
all developed countries, cigarette smoking has been the dominant form of
tobacco consumption for over 100 years.
Sweden is a remarkable exception.
Smoking rates among men in Sweden have always been lower than in any
other developed country, resulting
in the lowest rates of lung cancer – indeed, of all smoking-related deaths. The reason is
that, instead of smoking, Swedes enjoy nicotine and tobacco by using snus, a 200-year old smokeless product.
A
study published in the Scandinavian Journal
of Public Health examined lung cancer – the sentinel disease of smoking – among
men and women in all European Union countries.
It concluded “that snus use is inversely correlated with cigarette
consumption among men in Sweden, resulting in the lowest [lung cancer mortality
rates] in Europe for most of the past 50 years.”
Numerous published studies have documented that male smokers in
Sweden have used snus as a gateway to a smoke-free life, but that is only part
of the story. Snus use has also played a
valuable role in steering tobacco initiators away from cigarettes. Any tobacco use among children should be
discouraged, but Swedish boys who experiment with tobacco choose snus, the product their fathers use. This fact is well-received by tobacco
research and policy experts who focus on eliminating deaths from smoking, not
on eliminating tobacco.
With
respect to tobacco, Sweden is unique in the 28-country EU, which bans snus
everywhere else. The effect of this
prohibition is profound. If men in all
EU countries had the smoking rate of Swedish men, nearly 300,000 deaths from smoking could be avoided each
year.
The
Swedish experience also has implications for its neighbors Norway and
Finland. In 1995, when Sweden and
Finland joined the EU, Sweden applied for and received a waiver on the EU’s
existing snus prohibition, thereby allowing Swedes to continue producing and
selling within the country. Finland
adopted the ban, and since Norway never joined the EU, snus remained available
there.
Norwegian
tobacco research experts have documented that snus suppressed smoking rates there.
In Finland, the decline in smoking levelled off after the 1995 snus ban, while the
decline in Sweden continued.
The
Swedish experience wasn’t launched as a government program or anti-tobacco
campaign. It arose organically as
tobacco users in Sweden made rational choices to use snus instead of
cigarettes.
Dr. Robi: If you had to state a clear
message to the public about smokeless tobacco, what would it be?
Dr.
Rodu and Dr. Nitzkin: The Swedish experience exemplifies harm reduction:
consumers making rational choices to use smokeless instead of cigarettes, based
on accurate perceptions and preferences.
The 40-50 million Americans who consume tobacco deserve truthful
information from government and health organizations about vastly safer
smokeless tobacco, e-cigarettes and vapor.
Millions of them could make the switch from combustible to smoke-free
and lead longer and healthier lives. How
Swede it could be.